Abstract
The serum free light chains (sFLC) assay provides a minimally invasive method for probing plasma cell clonality and has clinical value in diagnosing, monitoring, and prognosticating patients with monoclonal gammopathies (MGs). sFLC interpretation involves the calculation of the kappa to lambda sFLC concentration ratio (sFLC-ratio). An abnormal sFLC-ratio can provide evidence of a clonal plasma cell process. However, the sFLC-ratio is prone to false positives in patients with impaired renal function (IRF). To address this problem, prior studies have proposed renal specific reference intervals for use in patients with IRF, defined as an estimated glomerular filtration rate (eGFR) less than 60 mL/min/1.73m2. This solution has several important limitations. First, a contemporaneous eGFR result is required to identify which reference interval should be reported. Second, the cutoff of 60 mL/min/1.73m2 is arbitrary and not data-driven. Third, performing multiple reference interval studies poses a major cost barrier. Finally, most laboratory information systems (LIS) do not support the use of multiple reference intervals for a single discrete result. The overall goal of this study was to provide a practical solution to improve the diagnostic utility of the sFLC assay for patients with IRF.
The LIS and electronic health records of Barnes Jewish Hospital (BJH, St. Louis, MO) were queried to retrieve all sFLC results, sFLC-order associated diagnosis codes, serum immunofixation electrophoresis (IFIX), serum protein electrophoresis (SPEP), and Creatinine (Cr) results between 01/01/2019 and 01/01/2022. sFLC and Cr results were matched based on closest collection time. For patients with multiple paired sFLC/Cr results the earliest set was retained leaving 5,542 pairs of unique patient results. eGFR was calculated using the 2021 CKD-EPI formula. A non-MG cohort of 413 patients was defined based on a negative IFIX and the absence of an order-associated diagnosis code of an MG. In addition, an MG cohort was defined comprising 1,296 patients with a paraprotein on IFIX or SPEP and an order-associated ICD10 code of an MG.
It was observed that 46.1% of patients subjected to sFLC testing had IRF. Among non-MG patients, those with IRF had a significantly greater median[IQR] sFLC ratio compared to those without IRF, 1.7[1.36-2.16] versus 1.29[1.03-1.56] g/dL (p<0.001 by Wilcoxon rank sum test). In addition, the MG false positive rate of the sFLC-ratio was significantly greater among those with IRF, 52.9% versus 19.6% (p<0.001 by Chi-square test).
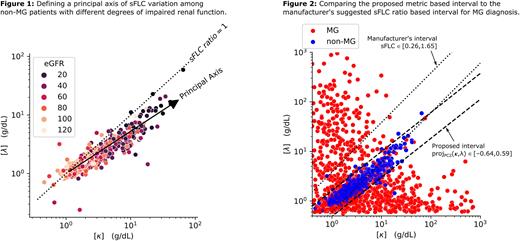
Next, using principal component analysis, a new metric was defined that represents distance from the principal axis of variation in kappa and lambda concentrations among non-MG patients (Figure 1). A diagnostic interval was defined for this metric (-0.64 to 0.59) using the 2.5-97.5% range of the distribution observed among non-MG patents. Visual inspection suggested the new interval separated the data from the MG and non-MG cohorts better than the manufacturer's sFLC-ratio based interval (Figure 2). The novel metric had significantly improved specificity overall (94.7% vs 63.5%, p<0.001) as well as among patients with IRF (91.7% vs 46.4%, p<0.001).
Consistent with prior studies, this work provides evidence that IRF is common among patients tested using the sFLC assay and is associated with poor diagnostic specificity of the sFLC-ratio. We describe a novel metric and demonstrate its use for improving the diagnostic specificity of the sFLC assay. An attractive feature of our approach is that it can be implemented with a single diagnostic interval because the metric presented is robust to variation in renal function.
Disclosures
Brestoff:Burrough Wellcome Fund: Research Funding; Springer Science + Business Media: Patents & Royalties: Royalties; DeciBio: Consultancy; Flagship Pioneering: Consultancy; American Society for Clinical Investigation: Honoraria. Jackups:Werfen: Consultancy; Wiley and Sons: Other: Educational Grant. Zaydman:Siemens Healthineers: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal